Harmony Health Group Accepts UHC Insurance
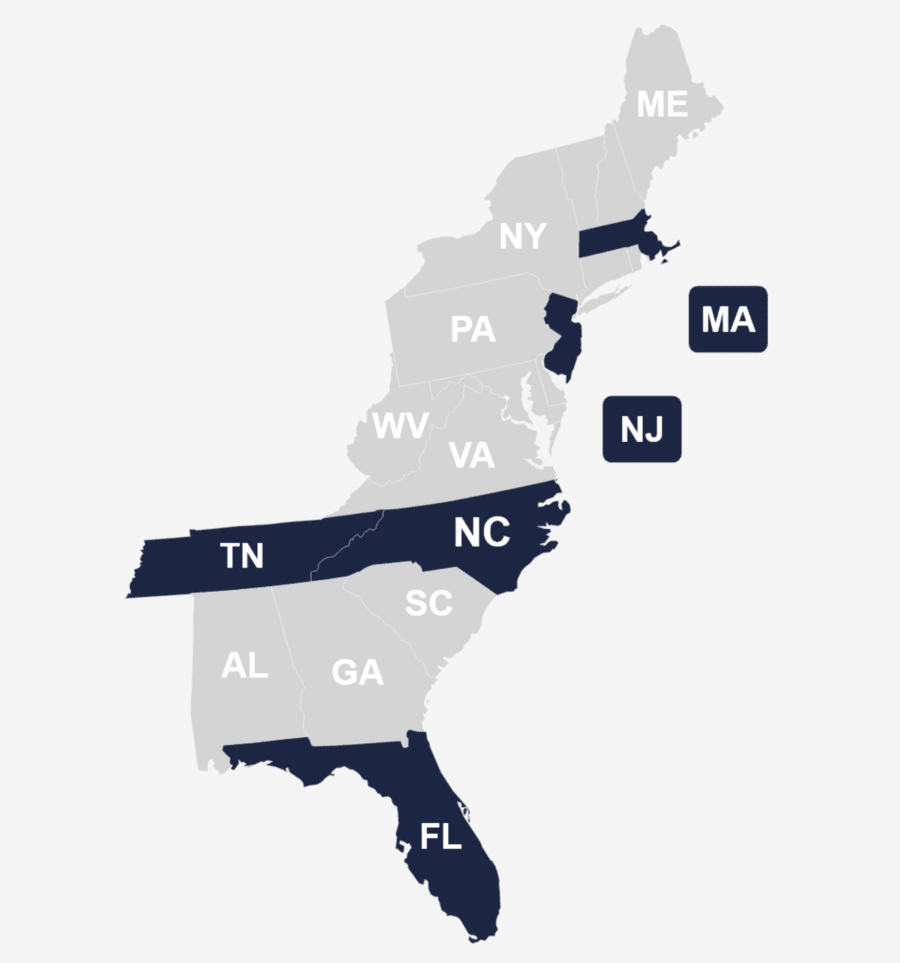
Harmony Health Group operates multiple rehabilitation centers across Florida, Massachusetts, North Carolina, New Jersey, and Tennessee, offering comprehensive care for substance abuse and mental health challenges. In-network with various insurance providers, including United Healthcare (UHC), Harmony Health Group accepts insurance for substance abuse, mental health, and dual diagnosis treatments.
This accessibility ensures individuals with UHC coverage can access quality rehabilitation services, making the path to recovery more feasible. Harmony Health Group provides reliable support across multiple states if you’re seeking rehab centers that take UHC. Below, uncover all you need to know about leveraging your United Health Care Insurance to support quality addiction treatment near you.
Check Your UHC Coverage Levels with Harmony Health Group
You can check your insurance coverage levels by calling us on: (866) 461-4474
We’re here to listen. Let’s talk today.
What is United Health Care Insurance Drug & Alcohol Rehab Coverage?
United Healthcare rehab coverage provides comprehensive health benefits for substance abuse and addiction, encompassing mental health treatment and behavioral health services. This coverage may extend to in-network inpatient or outpatient care, detoxification, therapy sessions, medication-assisted treatment (MAT), and more.
For a detailed overview of your insurance benefits for United Healthcare alcohol rehab or United Healthcare drug rehab, call (866) 461-4474.
Does United Healthcare Cover Mental Health Treatment Near Me?
UnitedHealthcare (UHC) includes mental health therapy treatment in its health insurance plans as mandated by the Affordable Care Act (ACA), with coverage falling under essential health benefits. Within UHC, mental health treatment may include substance abuse services, acknowledging the growing importance of comprehensive care amid increased mental health awareness.
To meet diverse mental health needs, UHC offers various resources and support to address a broad range of conditions, including access to a network of professionals like psychiatrists, psychologists, counselors, and therapists, with the option of telehealth sessions for added convenience. Coverage specifics may vary, so review your plan documents, contact United Healthcare directly, or call (866) 461-4474 to connect with one of our representatives at Harmony Health Group, who can clarify your mental health insurance coverage details.
Some Various UHC Insurance Brands, Products, & Services
Does UHC Cover Rehab for Drug Abuse and Alcoholism?
Yes, United Healthcare typically covers rehabilitation services for drug abuse and alcoholism. These services include both inpatient rehab and outpatient care options, offering comprehensive recovery support. UHC recognizes the importance of addressing substance abuse and providing coverage for counseling, therapy, and evidence-based treatments.
To fully understand your benefits, reviewing your policy details for factors like treatment duration and in-network options is essential. UnitedHealthcare and Harmony Health Group are dedicated to supporting individuals on their recovery journey by offering accessible, comprehensive coverage for rehabilitation services. Call (866) 461-4474 to learn more and gain precise details on how your coverage applies to your needs.
Does UHC Cover Medical Detox Treatment?
UnitedHealthcare typically covers medical detoxification treatment, an essential step in addiction recovery. This supervised process, overseen by medical professionals, ensures safe withdrawal from addictive substances. While coverage specifics may vary, you can check your UHC insurance plan for details on factors such as treatment duration and inpatient care options.
Contact Harmony Health Group for assistance navigating your insurance details. Call (866) 461-4474.
Harmony Health Group’s Drug & Alcohol Rehab Center Locations
In the journey to conquer addiction and maintain lasting sobriety, Harmony Health Group stands as a committed ally, offering compassionate care and personalized solutions. Explore the treatment locations listed below, and feel free to reach out at (866) 461-4474 for more details and customized guidance to start a healthier chapter in your life.
Treatment Centers in Florida (FL) That Takes UHC Insurance
Treatment Centers in Massachusetts (MA) That Take UHC Insurance
Treatment Centers in North Carolina (NC) That Take UHC Insurance
Treatment Centers in New Jersey (NJ) That Take UHC Insurance
Treatment Centers in Tennessee (TN) That Take UHC Insurance
Harmony offers a multitude of locations up and down the East Coast for behavioral health services. Call us to learn about our facilities and treatment options.
Does UHC Insurance Cover Residential Treatment?
If you’re looking into residential treatment, United Healthcare (UHC) insurance typically covers it to provide you with the intensive support it provides. This level of care is recommended for more particularly challenging situations related to substance use or mental health disorders. UHC offers coverage for services such as individual and group therapy, medical monitoring, and holistic interventions.
Keep in mind that coverage specifics may vary, so it’s essential to review your plan details, including factors like treatment duration and in-network facilities. For a comprehensive grasp of your specific coverage details, carefully examine your UHC policy or reach out to our team at (866) 461-4474 for personalized assistance and guidance.
Does UHC Insurance Cover Eye Movement Desensitization and Reprocessing (EMDR) Therapy?
Yes, UnitedHealthcare (UHC) insurance typically covers Eye Movement Desensitization and Reprocessing (EMDR) therapy, which is recognized as an evidence-based therapeutic approach particularly effective for treating trauma and post-traumatic stress disorder (PTSD). UHC’s coverage for EMDR reflects its commitment to providing diverse and effective mental health interventions for its members.
EMDR therapy involves a structured eight-phase approach that includes recalling distressing memories while engaging in bilateral stimulation, such as guided eye movements. This process aims to help individuals process traumatic experiences and alleviate associated symptoms. While UHC’s coverage for EMDR is generally comprehensive, individual plans may have specific details and variations in coverage. If you’re considering EMDR therapy, review your insurance plan details, including any copayments or out-of-pocket expenses associated with this treatment. Contacting UnitedHealthcare directly or calling (866) 461-4474 can provide more precise information on your coverage.
Does United Healthcare Cover Mental Health Therapy Treatment?
Yes, United Healthcare (UHC) generally covers mental health therapy, including inpatient and outpatient care. These services encompass various therapeutic interventions, such as motivational interviewing, for conditions such as depression and anxiety. Coverage specifics will vary according to several influencing factors, like the services provided and your particular insurance plan.
Call (866) 461-4474 to review your UHC plan for details like copayments, deductibles, limitations, and exclusions. Having a clear understanding of your mental health therapy coverage leads to more informed decisions regarding the appropriate and necessary care.
Mental Health Therapy Programs Covered by UHC
How To Check United Healthcare Insurance Coverage Levels for Addiction Treatment Near Me
For personalized assistance in checking your UnitedHealthcare (UHC) insurance coverage levels for addiction treatment, we invite you to connect with us directly. Our dedicated team is here to guide you through the process, offering friendly and professional support to help you understand your coverage details. Give us a call at (866) 461-4474 to speak with one of our representatives today.
Alternatively, you can conveniently verify your insurance coverage by completing our online form linked below. Follow the simple steps to gain clarity on your UHC insurance coverage levels for addiction treatment. We strive to ensure a smooth and effortless experience, equipping you with the necessary information to start your path to recovery confidently and with a sense of tranquility.
Verify Insurance at: https://www.harmonyrecoverygroup.com/insurance/
Other Addiction Treatment Programs Covered by UHC Insurance
UnitedHealthcare (UHC) broadens its coverage to include personalized rehabilitation programs to address each person’s needs. Embracing a comprehensive strategy that surpasses conventional treatments, UHC provides alternative, all-encompassing therapies and tailored programs. Below is a brief overview of the treatment options aligning with UHC’s dedication to fostering well-being and the journey to recovery.
UHC Insurance Coverage for Inpatient Rehab
UHC Insurance Coverage for Intensive Outpatient Program (IOP)
UHC Insurance Coverage for Partial Hospitalization Programs (PHP)
UHC Insurance Coverage for Acute Treatment Programs
How Much is Rehab with UHC Insurance?
Navigating the cost of rehab with United Health Care (UHC) insurance is a personalized journey influenced by factors such as your specific plan details and the type of rehab program you choose. On average, drug rehabilitation expenses per individual total $13,475. Call (866) 461-4474 to understand out-of-pocket costs, deductibles, copayments, and other policy specifics.
Harmony Health Group is dedicated to supporting your recovery journey. Don’t hesitate to reach out for a tailored understanding of the costs associated with rehabilitation under your UHC benefits, customized to your specific treatment needs. Our team is here to provide professional, transparent, and friendly assistance, guiding you through the financial aspects of your recovery journey.
How To Get UHC Insurance to Pay for Drug & Alcohol Rehab Treatment
Embarking on the journey toward recovery from the challenges of drug and alcohol addiction is a significant stride. To secure coverage for rehab treatment, consider these actionable steps. First, contact UHC customer service or connect with Harmony Health Group at (866) 461-4474. Our team is ready to communicate with your insurance provider on your behalf.
Delve into the details of your policy by thoroughly reviewing the documents and understanding essential aspects like deductibles, copayments, and limitations. Choose the supportive environment of in-network rehab centers that take UHC to reduce out-of-pocket expenses. Verify coverage for your intended treatment options, be it inpatient or outpatient care, counseling, detoxification, or medication-assisted treatment (MAT). If prior authorization is needed, collaborate with your healthcare provider to obtain approval before starting rehabilitation. Maintain meticulous records of all communications with UHC and your treatment providers. Leverage UHC’s online resources through its website or member portal for a deeper understanding of your coverage. This strategic, mindful approach empowers you to confidently navigate the process, fostering clarity and assurance throughout your pursuit of healing and recovery. For any challenges or queries, our team at (866) 461-4474 is here to provide personalized guidance and assistance.
National Statistics on Drug & Alcohol Rehab and UHC Health Insurance Claims
Get in touch with Harmony Health Group to find out about our rehab admissions process, free assessment, treatment options or to check your insurance coverage levels. Your first step to recovery starts here!
Provide Your Contact Details
8520 Cliff Cameron Dr. Ste 450, Charlotte, NC 28269
